The Healthy Start MomCare Network, Inc. is an administrative service organization representing all Healthy Start Coalitions under the provisions of s.409.975(4)(a), F.S.
The Network is tasked with implementing services provided to Medicaid participants during pregnancy and after delivery under the state’s federal Medicaid waiver. The Network contracts with the state Agency for Health Care Administration (AHCA) and the coalitions to establish specific programs and procedures to improve pregnancy outcomes and infant health among Medicaid recipients, including, but not limited to, coordination with the Healthy Start program, immunization programs, and referral to the Special Supplemental Nutrition Program for Women, Infants and Children, and the Children’s Medical Services program for children with special healthcare needs. In addition, the Network coordinates with managed care plans in providing care for Healthy Start participants and monitors performance on specific measures to determine the adequacy, timeliness, and quality of services for pregnant women and infants.
How to Access Services
Healthy Start services may be accessed by completing Florida’s Prenatal Screen at a provider’s office, by referral through a community agency or managed care organization, or self-referral to CONNECT.
Learn more about Healthy Start and services available in your community by contacting your local Healthy Start Coalition, or calling 1.855.889.1090.
If you are enrolled in Healthy Start and have a complaint or concern, find out more about your rights and responsibilities here.
Our Notice of Privacy Practice has information on how medical information about you may be used and disclosed.
If you are not satisfied with your treatment or the services provided, you have the right to submit a complaint or grievance through your local Healthy Start Coalition or contact us here.
Learn more about Health Plans and Medicaid: https://www.flmedicaidmanagedcare.com/
Most Medicaid clients are required to enroll in a Managed Medical Assistance (MMA) plan for their medical services like doctor visits, hospital care, prescribed drugs, mental health care, and transportation to these services. This website will provide you the Medicaid Managed Care plans available in your geographical area, guidance about selecting an MMA plan and how to make a plan choice.
If a DCF Applicant for Medicaid does not select a plan they will be assigned to one if they are required to be enrolled in an MMA plan to receive Medicaid services. Please make your plan selection today so you can be enrolled in the plan that best meets your needs when you are determined eligible.
News
- RFP#2024-02: Florida Association of Healthy Start Coalitions and Healthy Start MomCare Network, Inc. Request for Proposal for Financial Statement Audit Services Questions and Answers July 22, 2024Download Questions and Answers Download HSMN Audit Download FAHSC Audit Download FAHSC communication letter Download HSMN communication letter Download FAHSC 990 Download HSMN 990Read more ...
- ITN#2024-01: Healthy Start MomCare Network, Inc. Invitation to Negotiate Statewide Data System Timeline Revision June 7, 2024Download TimelineRead more ...
- ITN#2024-01: Healthy Start MomCare Network, Inc. Invitation to Negotiate Statewide Data System Public Notice for ITN Proposal Review Meetings–UPDATED May 14, 2024
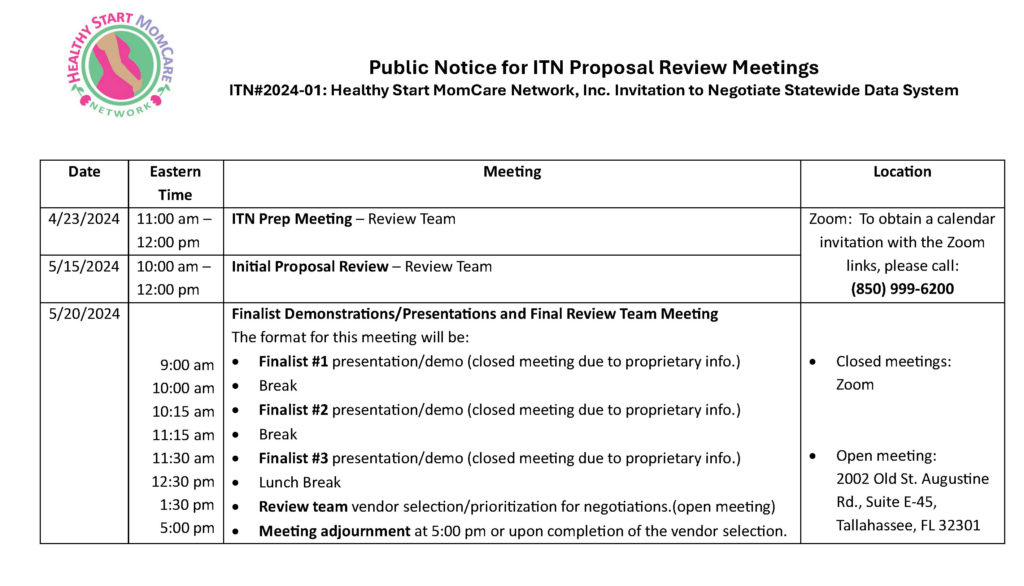 Download Meeting scheduleRead more ...
Download Meeting scheduleRead more ... - ITN#2024-01: Healthy Start MomCare Network, Inc. Invitation to Negotiate Statewide Data System Initial Review of ITN Proposals May 13, 2024Rescheduled Proposal Opening HSMN ITN 2024-01 Statewide Data System When: May 15, 2024 10:00 AM – 12:00 PM AM Eastern Time ...Read more ...
Board Members
Public Meeting Notice
Click on the links below for agendas and webinar information when available.
- SU
- MO
- TU
- WE
- TH
- FR
- SA
- 30
- 1
- 2
- 3
- 4HSMN Finance Committee Mtg11:30 am - 12:30 pmRegister in advance for this meeting: https://us02web.zoom.us/meeting/register/tZcofumorzwpHNIjg3dZAbfLZ5Z0vz0zh7V5 , ...
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12HSMN Provider Update Mtg10:00 am - 11:00 amRegister in advance for this meeting: https://us02web.zoom.us/meeting/register/tZwkfuuuqjwvHtce0onNGoeoLaTFmJy_3OB2 , ...
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 1
- 2
- 3
Reoccurring Meetings
Auditors’ Reports
FYE 2022 HSMN Financial Statements and Independent Auditors’ Reports
HSMN Form 990











