
Working to Increase Service Delivery for Florida Families (2022-24)
We are very thankful for the increased funding from the legislature that began in July 2023. Prior to this, Healthy Start funding for non-Medicaid eligible families had not been increased for more than 17 years. Since then, the cost of providing services has increased 51%. Healthy Start Coalitions are struggling to meet the needs of these families and adequately pay for the workforce needed to support these services. In the last four years, we have seen a significant increase in the number families being served who are not eligible for Medicaid (132% increase in home visiting and 47% Coordinated Intake and Referral). With the end of the Public Health Emergency, we anticipated 7% more families will shift from Medicaid to non‐Medicaid. For this reason, Florida Association of Healthy Start Coalitions is asking the Florida Legislature for a funding increase. Click here and here to learn more.

Addressing the Critical Need for More Fatherhood Programs in Florida (2021-22)
We are grateful to the legislature for the huge investment in services for fathers in Florida including Healthy Start’s T.E.A.M. Dad program that began in January 2023. There is a father absence crisis in America. According to the U.S. Census Bureau, 18.3 million children, 1 in 4, live without a biological, step, or adoptive father in the home. This same research shows that when a child is raised in a father-absent home, he or she is at a 4x greater risk of poverty; 7x more likely to become pregnant as a teen; more likely to have behavioral problems; more likely to face abuse and neglect; more likely to abuse drugs and alcohol; more likely to go to prison; 2x more likely to suffer obesity; more likely to commit crime and 2x more likely to drop out of high school. Additionally, infant death within the first 28 days of life is 4x higher for those with absent fathers than those with involved fathers. However, children with involved dads have better overall emotional and social well-being; are less likely to be mistreated; do better in school; and are less likely to carry guns. Boys have fewer behavior problems and girls have fewer psychological problems.
Click here to read more.

Fetal and Infant Mortality Review Program (FIMR)(2021-22)
We are extremely appreciative of the legislature’s support for the health of mothers in Florida by providing funding for the implementation of the Fetal and Infant Mortality Review Program (FIMR). Infant mortality is a sentinel indicator of the overall health and well‐being of a community and is defined as the death of an infant during the first year of life. Fetal mortality refers to a still birth that is at least 20 weeks or more gestation.
Both infant and fetal mortality are complex with many risk factors impacting the outcomes which is why FIMR programs are so important in helping to determine the causes of these deaths. Learn more here.
Improving Outcomes for Mothers & Babies: Infant Mortality in Florida (2021-22)
Infant mortality rate is often used as an indicator to measure the health and well-being of a community. Infant mortality is the death of an infant during the first year of life and is calculated as the number of infant deaths per 1,000 live births. Infant mortality is further classified into neonatal deaths which occur during the first 27 days of life and post-neonatal deaths which occur from 28-364 days of life.
Click here to read more.
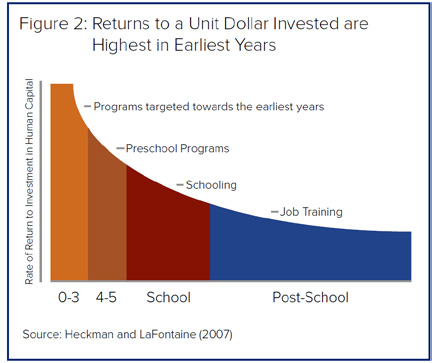
Investing in a Healthy Start for Florida’s Children (2020-21)
In a tight budget year, it is vital to remember that the highest rate of return on investment is during the earliest years (ages 0-3) . This is why it is critical to ensure that every baby has a chance at a Healthy Start.
Click here to read more.
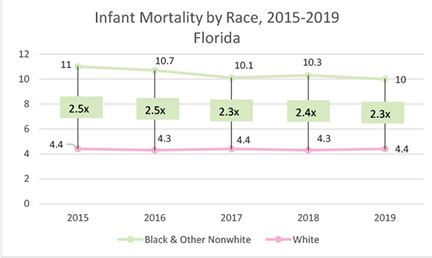
Racial Disparities in Birth Outcomes (2020-21)
Prematurity is a leading cause of infant deaths in Florida and across the country, and can lead to life-long health issues for infants that survive. There are also considerable racial disparities in premature birth –the preterm birth rate. In Florida, the preterm birth rate among black women is 52% higher than the rate among all other women.
Click here to read more.
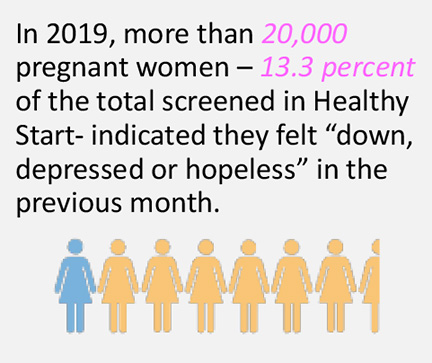
Perinatal Depression (2020-21)
Pregnant women with depression are 3.4 times more likely to deliver preterm and four times as likely to deliver a low birth-weight baby than non-depressed women. Perinatal depression also contributes to long-term health and developmental issues in children. Children of depressed mothers are at higher risk of experiencing development delays at 18 months, and physical health problems in early childhood, resulting in later social and emotional problems during adolescence and adulthood.
Click here to read more.

Maternal Mortality (2020-21)
Around 700 women die annually in the United States as a result of pregnancy or delivery complications. The maternal mortality rate has increased from 12.7 per 100,000 in 2002 to 17.4 per 100,000 in 2018. Black mothers in Florida are 2-3X more likely to die from pregnancy-related causes than White mothers.
Click here to read more.
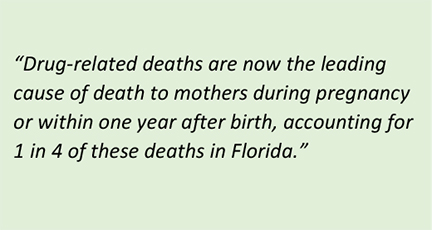
Substance Use Disorder (2020-21)
An estimated five percent of women — or more than 11,000 in Florida — use one or more addictive substances during pregnancy. Smoking tobacco or marijuana, taking prescription pain relievers, or using illegal drugs during pregnancy is associated with poor birth outcomes, including stillbirth.
Click here to read more.
Enhancing Medicaid Benefits 12 Months Postpartum (2020-21)
We are extremely appreciative of the legislature’s support for the health of mothers in Florida by approving the extension of Medicaid benefits for 12 months postpartum. According to the Perinatal Periods of Risk research, most fetal and infant deaths are due to the health of the mother before she gets pregnant. Currently, women in Florida who qualify for Medicaid due to pregnancy lose their coverage 60 days after their pregnancy ends leaving them uninsured until their next pregnancy and unable to address ongoing health issues such as hypertension. While current coverage allows for a postpartum visit (usually at six weeks), many pregnancy-related complications arise beyond this period.
Click here to read more.
